The following article was first published as a two-part series in the CovidX Digest on April 23 and April 30, 2020. CovidX, a Luminary Labs initiative, seeks to identify opportunities for government and the private sector to accelerate meaningful innovation that addresses COVID-19 and future pandemics. Sign up to receive updates.
Part 1: Antibody testing and why it matters
To tackle the coronavirus pandemic, we need to track prevalence, identify effective treatments, and protect ourselves from infection. In the absence of these solutions, we’re left with only blunt mitigation tools like statewide shutdowns. Antibodies may hold the key to tracking, treatments, and prevention — more precise tools for a “smart restart” — and that’s why leading institutions have pivoted to advancing our understanding of coronavirus antibodies and investing in potential solutions.
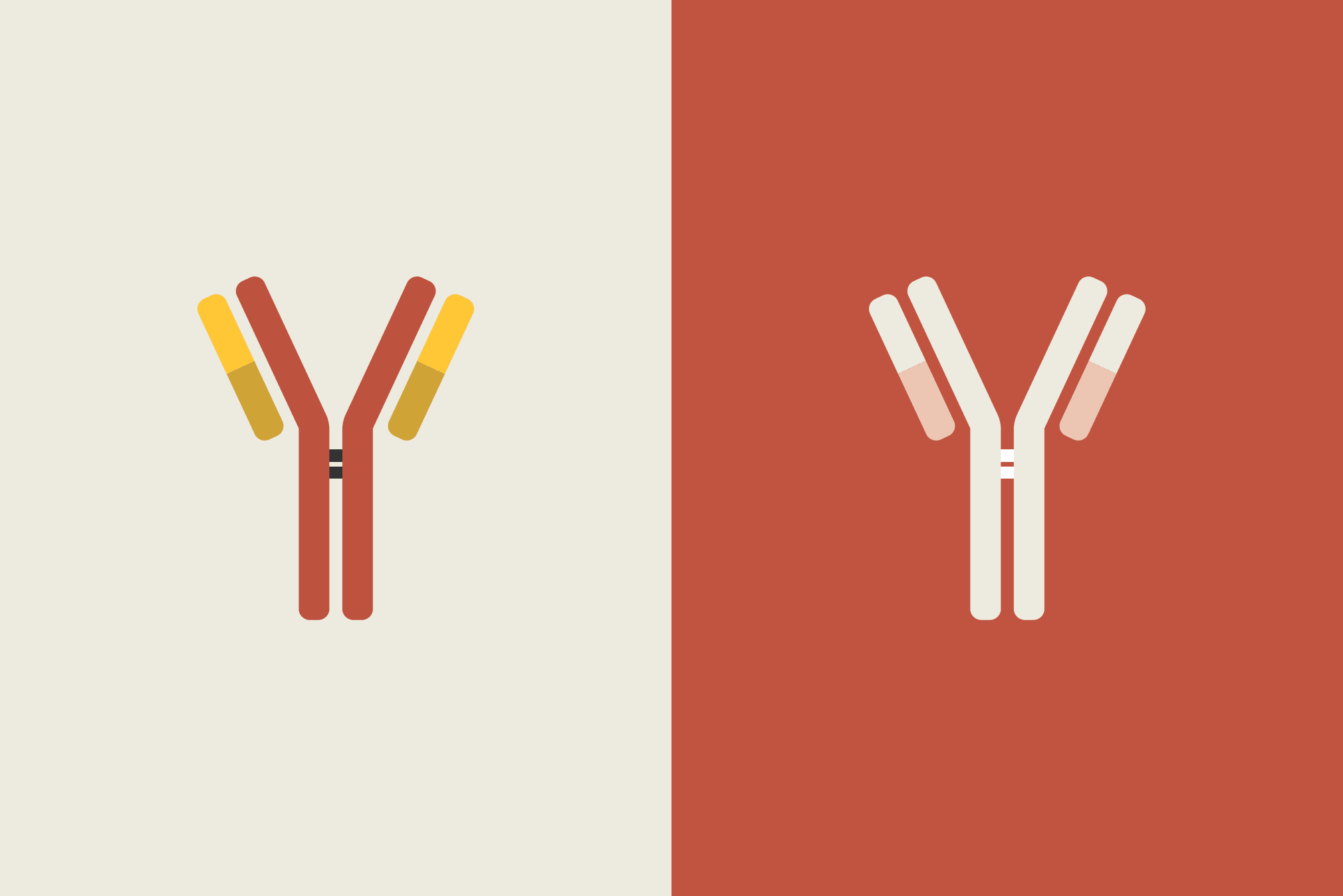
Antibodies are Y-shaped proteins produced by plasma and used by the body’s immune system to neutralize pathogens like viruses. The body forms different types of antibodies in response to viruses, including SARS-CoV-2: immunoglobulin M (IgM) and immunoglobulin G (IgG). IgM antibodies are formed during early stages of infection, and IgG antibodies take longer to form; a positive IgM test indicates recent exposure to the virus and early stages of infection, and a positive IgG test indicates a past infection and perhaps some level of immunity.
What we can learn from antibody tests
Antibody tests aren’t new; they have long been used to detect viruses like HIV, hepatitis, and measles. In the case of the novel coronavirus, antibody testing has several potential benefits.
Antibody testing allows us to see how many people have had the virus, which establishes a baseline for understanding spread, recovery, and fatality rates. We learned this week that the virus was spreading in the United States much earlier than previously thought; widespread antibody testing can help us figure out how many people have been exposed. It will also reveal the prevalence of asymptomatic infection and give us a more accurate idea of how deadly COVID-19 is.
Some tests allow us to see levels of different antibodies in people; experience with other viruses suggests that people who have recovered from COVID-19 will have immunity, but this has not yet been proven and we don’t yet know how long immunity might last. And finally, testing helps identify people who can donate convalescent plasma as a possible therapeutic.
Developing an accurate test
This virus is new, and so are the serological tests that screen for antibodies. What normally takes years is happening in a matter of weeks or months, and the urgency to make these tests available has resulted in a (likely temporary) tradeoff on quality.
To fast-track the development of antibody tests, the FDA has issued four Emergency Use Authorizations as of April 18, 2020. The agency will not object to the development and sale of tests that identify antibodies to SARS-CoV-2 where the test is validated, notification is provided to the FDA, and requisite information is provided — including a statement that the test is not FDA approved. To date, more than 90 companies have notified the FDA and released antibody tests. These are the early days of antibody testing; competition is likely to produce winning solutions.
Scaling access
Scientists are confident that they’ll be able to develop a viable test soon; the hard part will be making sure everyone can access testing. The profound scale of the pandemic means that antibody testing will need to happen at an unprecedented scale — and many people will need to be tested frequently. That means millions of daily or weekly tests for the foreseeable future, since that’s the only way to find out if antibodies provide long-term immunity.
Drawing blood is an invasive process that only trained professionals should do; less invasive, point-of-care and at-home testing could help scale efforts. Some labs have started offering finger-prick capillary tests, but the largest manufacturer of these tests reports accuracy rates as low as 61.8%, which will yield many false positives and false negatives.
As we’ve seen with virology testing, scaling is difficult. Expect to see similar supply chain issues — including shortages of test tubes, reagent chemicals, alcohol wipes, and PPE, as well as skilled phlebotomists and lab technicians who can draw blood and process tests.
Assuming we can predict and mitigate supply and labor needs, logistics will also be a consideration. If an entire population needs to be tested, someone will need to decide who gets tested first and how the bills for testing will be paid. If tests are done at home, someone will need to deliver them; if tests are done in person, clinics will need to figure out how to handle surges in volume.
Given the public health utility of antibody testing data, governments should give careful consideration to how samples are collected, saved, and used; that includes clarifying privacy protections for patients and security protections for data.
What’s happening now
Officials are suggesting that lifting social distancing restrictions will be contingent upon several factors, including antibody testing. A National Institutes of Health-funded antibody survey is enrolling 10,000 volunteers from around the country, and New York State began an antibody testing survey this week. Preliminary results from a random test of 3,000 people are in; an estimated 13.9% of New Yorkers have likely had the coronavirus. If this test accurately reflects incidence, that would mean 2.6 million New Yorkers have been infected — far greater than the 250,000 cases confirmed by virology testing. This type of data could dramatically change understanding of the COVID-19 death rate and help states make more informed decisions about the risks of reopening.
Part 2: Treatment, prevention, and scaling solutions
This week, all eyes are on September. Projections point to the pandemic curve slowly tapering off this summer in the United States, coinciding with the start of the school year and workers returning to jobs. But the flu season will be just beginning in the fall, and some fear a second wave of coronavirus outbreaks. Without careful planning, September might look a lot like February.
Antibody testing and planning for a “smart restart”
We already have a sense of the data we’ll need to make accurate projection models and plan for a “smart restart.” Diagnostic testing and contact tracing will need to scale up in a big way. We’ll need real-time, actionable views of hospital capacity and isolation facilities. And we’ll need baseline data for understanding spread, recovery, and fatality rates; antibody testing is critical.
Antibody tests can also reveal how many people might be protected from future COVID-19 infections and may be eligible to donate convalescent plasma. Not all infections result in immunity — for that, the body needs to produce a neutralizing IgG antibody, which prevents the virus from entering cells. Based on our understanding of other viruses, scientists believe a positive IgG antibody test may indicate some level of immunity from SARS-CoV-2, the virus that causes COVID-19.
Early results from New York’s antibody testing survey show that 14.9% of the state’s population have antibodies; the rate is higher in New York City, but still nowhere near the 70-90% required for herd immunity. Allowing the virus to spread in an effort to achieve this level of population immunity would result in millions of deaths — a risky trade-off that many states and countries are not willing to make. For a smart restart, we need more ethically palatable solutions.
Antibodies for treatment
Even the most optimistic experts tell us a vaccine is likely at least a year away, making finding an effective treatment against COVID-19 all the more important. While early results from antiviral drug trials are promising, we’ll need a range of treatment options. Antibody therapeutics have been described as a “bridge to a vaccine” and offer hope for treatment.
Researchers are experimenting with the use of antibody therapeutics to treat severely ill patients. Convalescent plasma therapy, which involves a transfusion from a recovered patient with antibodies, has been used to treat measles, H1N1, and even the Spanish Flu in 1918-19. Early studies show positive results for COVID-19, and the FDA has authorized its use in clinical trials and emergency cases.
An alternative to convalescent plasma is the use of hyperimmune globulin, which involves pooling plasma samples and then purifying and incubating large batches over several weeks. This is safer — it reduces the risks of transmitting other bloodborne viruses — and more potent than convalescent plasma.
Even as more people recover from infection and develop SARS-CoV-2 antibodies, we still won’t have enough plasma to treat everyone who’s sick. We need scalable solutions.
Researchers around the world have been sequencing the virus genome and identifying antibody candidates. Normally this process takes years — but frontier technologies are accelerating discovery. For example, the Crowe Lab at Vanderbilt University has identified thousands of antibody candidates and is on the path to testing and manufacturing. The first human trials could happen as early as this summer.
A number of pharmaceutical companies — including GlaxoSmithKline, AstraZeneca, Takeda, Eli Lilly, and Regeneron — are developing treatments now with the hope of testing them in the next few months.
Antibodies for prevention
Preventing infection and illness is important, especially when a smart restart requires reducing the burden on healthcare systems. Researchers are studying whether antibodies can be used as a prophylactic to prevent people contracting COVID-19.
The goal of prophylactic immunization is to prevent the establishment of infection; for virus infections, that means preventing viral entry into host cells. Unlike a vaccine, which prompts an immune system response and takes some time to develop, a passive antibody therapy could provide immediate, if short-lived, immunity. While most vaccines create long-term and sometimes permanent immunity, antibody prophylactics only create immunity for several weeks or months. In the context of COVID-19, antibody prophylactics are sometimes viewed as a possible “temporary vaccine” for high-risk populations — such as vulnerable individuals with underlying medical conditions, frontline workers, or people with exposure to confirmed cases of COVID-19.
While addressing the current pandemic is the most urgent need, broad-spectrum solutions might also help us fight the next outbreak. For example, Distributed Bio is looking for antibodies that have worked against other coronaviruses and could be engineered to adapt to the new coronavirus. If this approach to antibody engineering and universal vaccine design works, we’ll be better positioned to respond to future pandemics.
Planning for the fall
There are more discoveries to be made and challenges to overcome. However, we’ve spoken with experts who express a high level of confidence in arriving at antibody solutions within just a few months. But science alone isn’t enough to make these solutions a reality.
We will need widespread antibody testing, in addition to diagnostic testing, to better understand the spread of the virus, and figure out a population’s level of immunity in a given area. And we’ll need to develop a strategic plan for the development, manufacturing, and distribution of antibody therapies. Here’s what that plan should address:
- Shoring up the supply chain — What materials are needed for research, trials, and production? How will we deliver at scale while avoiding the logistics challenges we’ve already faced with testing and equipment?
- Prioritizing delivery — Assuming prophylactics won’t be available to the world’s 7.5 billion people at the same time, who will have first access to passive antibody therapies? (And who will make that decision?) Will frontline workers and vulnerable populations need to receive preventative therapies multiple times until a vaccine is available?
- Making care accessible — Who will pay for antibody testing and therapies? The virus doesn’t recognize borders, and no one will be safe from an infectious disease outbreak unless we take care of the most vulnerable. Manufacturers and governments will need to consider new financial models and intellectual property licenses to make testing, treatment, and prevention available to the entire world.
Adaptive systems enable more precise shutdown measures and more successful restart plans. With baseline antibody data and ongoing testing, we’ll understand how the disease spreads and which communities face the greatest risks. High-risk populations can receive prophylactic antibodies, and when there is an outbreak, we can isolate and treat those who are infected with antibody therapies.
It’s difficult to imagine what the future looks like, but it’s safe to bet that antibody solutions will be essential for helping us navigate the next two years. And if we get this right, we have a chance to get back to a better version of “normal” than we knew before.