Primary care is a hot topic again. Physicians are in short supply, and that’s not likely to change anytime soon. America’s population is aging, and as lifespans increase, we expect to see more instances of age-related disease states and comorbidities that strike later in life. Our needs for care will only increase. Technology — from mobile devices to artificial intelligence — may be poised to fill some of the gaps. But even when older patients adopt digital tools and behaviors, they still name doctors as their most trusted touchpoints. Healthcare is a human business, and people want to receive care from other people.
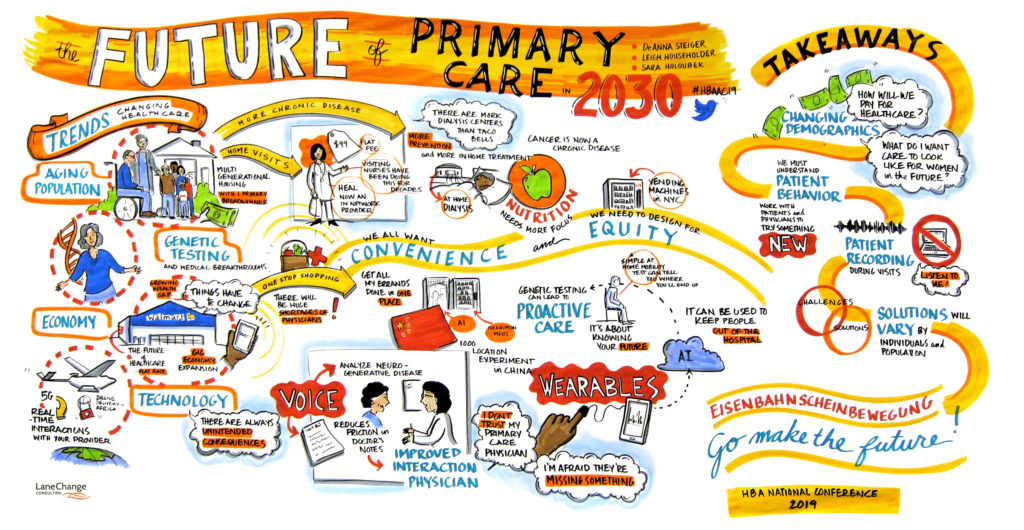
So how will we actually deliver primary care in the year 2030? At the HBA Annual Conference last month, I joined Syneos Health’s Leigh Householder, Amgen’s DeAnna Steiger, and illustrator Nevada Lane to explore four possible scenarios for the future of primary care.
Scenario 1: Home visits
In the 1930s, 40% of doctor appointments were house calls. This figure dramatically dropped in the last half of the 20th century; today, house calls account for only 1% of doctor visits. It’s less efficient for doctors to spend time traveling between appointments and transporting equipment. But with an aging population, the rise of hospital-acquired infections, and consumer preference for convenience, house calls are making a comeback.
Not unlike other modern, on-demand services, this level of care isn’t available to everyone. Heal, a startup that has partnered with Uber and Lyft, is operating in a few coastal metro areas — for now — but patients who have used the service report high levels of satisfaction. Superficially, home visits seem expensive. But CareMore’s “Home Team” model has reduced expensive hospital admissions and emergency room visits.
Scenario 2: The high-tech medical center
Medical breakthroughs and advancements in technology — from personal genomics to biometric monitoring to AI-powered everything — make it easier than ever to envision a highly effective and efficient outpatient setting.
Artificial intelligence and machine learning applications range from the administrative (e.g., predicting attendance) to the clinical (e.g., augmenting physicians). The rise in genetic sequencing presents great opportunity for what is known as precision medicine, enabling personalized care — from nutrition to cancer treatment — based on an individual patient’s genome. But not all patients are ready to talk to doctors about their DNA or share their genetic testing and other biometric data with insurance providers — and primary care facilities may not be ready to deal with the data, either.
Until clinicians and patients learn to communicate with and about AI and the data that powers it, the opportunity to transform healthcare will be unevenly distributed. There are many reasons to be optimistic about emerging technology in primary care, but it’s not yet clear what will be possible by 2030.
Scenario 3: The retail clinic
Walk-in clinics, once considered the least desirable option for primary care, found new relevance with the launch of QuickMedx (now CVS MinuteClinic) in 2000. Today, there are more than 1,100 MinuteClinics inside CVS and Target stores. And while underperforming CVS stores are closing, clinics are taking over as pharmacies become less about retail and more about providing healthcare.
More recently, retail clinics have inched closer to becoming the place of primary care, especially for those with chronic conditions. Walgreens, despite rumbles of a private-equity buyout and an announcement that it is closing 160 clinics, recently partnered with VillageMD to open the first of five new doctor-staffed primary care clinics in Houston. Walmart recently opened a stand-alone primary care facility in Georgia, turning heads with its breadth of services and its flat-fee model, even for the uninsured.
Scenario 4: Virtual care
Since the early days of the telephone and the golden age of radio, physicians have dreamed of using new communications devices to connect with patients. Today, increasing access to broadband internet, smartphones, and connected devices has resulted in a wider variety of telemedicine possibilities — from text and apps to virtual reality and voice assistants.
More modalities, of course, mean more startups. No single player is dominating the telemedicine market, and patients who visit different doctors may use multiple systems. Your employer-provided insurance may offer a voice assistant, your doctor may have an app, and when discharged from a hospital visit, you may use yet another virtual care solution.
Telemedicine isn’t just for elderly patients at home. Busy executives in the office and parents coordinating care for children also see the appeal of remote care. Hospitals benefit, too: Telemedicine extends services to nursing facilities and augments emergency care in remote locations.
For telemedicine to achieve its full potential, it must be integrated into larger systems. While integration of electronic health records has historically been an issue in telemedicine, that barrier is decreasing. Reimbursement, however, remains a challenge. Only 10 states have true telehealth payment parity, and others maintain laws that restrict telemedicine by not requiring insurance plans to cover telehealth services.
So which model will win? None of these scenarios are mutually exclusive. Elements of each will evolve — in predictable and unpredictable ways — and the way patients experience the future of primary care will depend on their ages, who they’re caring for, where they live, and what their conditions are.
Which scenarios are most likely? Which would you most like to see? Read more of Sara’s observations and join the conversation on LinkedIn.